A note on intraligamentary injections
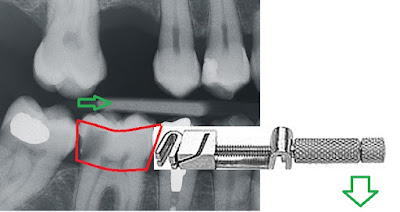
One thing I am never sure of during an intraligamentary injection is "is the needle tip in the PDL space or in the tissues?"Always use a small gauge needle even if you have a large gauge needle out for a block. A larger gauge needle will be too chunky to predictably fit into the PDL space. The angle of the needle is important and should be pointed towards the tooth surface. If it is inserted quite parallel o the tooth it will tend to sit in the gingival tissues and you will feel back pressure but will only be injecting into tissues with nothing reaching the periapical tissues. You may notice quite profound blaching in the area if you're inecting mainly into the tissues. In a thin biotype, it is quite easy for the needle to deflect away from the tooth and pierce the tissues back into the oral cavity. The best indication of a good needle placement is when you pull back, the needle tip is stuck in the PDL space and it is difficulty to remove. A patient with significant apica...