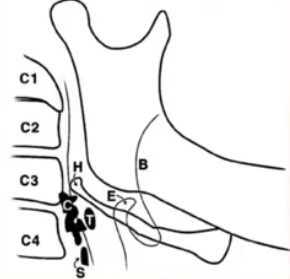
Cervical burnout
Currently trying to find out more information about cervical burnout (CB) and its differentiation from root surface caries (RSC) as I have had trouble distinguishing the two in the past. From what I can gather, -CB appears on the mesial and distal surfaces of teeth in the cervical region - It is a diffuse (ill defined) radiolucent (blacker) area and is bounded by the CEJ and the alveolar ridge -It may be due to overexposure of the film which can "burnout" the thinner sections of teeth. i.e there is lower absorption of the xrays by this anatomical area so if the exposure is high enough, the film in this area will totally "blacken". -It is optically more prominent due to the contrast with the adjacent radioopaque bone and enamel. -RSC has a similar radiolucent bowlshaped area on the radiograph. However, It will generally have a loss of tooth structure i.e in CB there is an intact tooth surface radiographically whereas this is not intact in RSC. Also, CB will sit