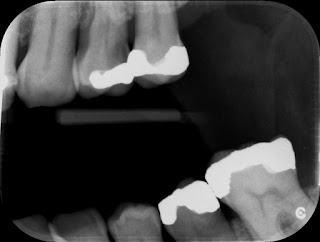
Restoration of endodontically treated teeth
Typically, root canal treatment is initiated because of deep caries or trauma, both of which often result in extensive loss of tooth structure. Additional tooth tissue is removed for endodontic access, cleaning and shaping of the root canal, and post space preparation, further reducing the structural integrity of the tooth and decreasing its resistance to fracture. At one time it was believed that endodontically treated teeth are inherently more brittle and susceptible to fracture. Subsequent research has shown that the dentin of endodontically treated teeth exhibits mechanical properties equivalent to that of untreated teeth. It has also been proposed that a portion of the sensory feedback mechanism is lost when the neurovascular tissue has been removed from the tooth in the course of endodontic therapy. Clinically, this means that the patient can inadvertently bite with more force on an endodontically treated tooth than on a vital tooth because of the impaired ...