Skip to main content
Leukoplakia and other White lesions
- Alveolar ridge keratosis
- White changes of the retromolar region or the alveolar mucosa where teeth have been extracted.
- Asymptomatic white, homogeneous discolouration of the mucosa
- Caused by direct irritation from foods against the edentulous ridge by opposing teeth
- Benign lesion. If believed to be alveolar ridge keratosis then no treatment other than follow up
- Aspirin burn
- Superficial burning of the oral mucosa due to the local application of aspirin or paracetamol.
- White, non wipeable discolouration of the mucobuccal fold, buccal mucosa or border of the tongue
- Cease drug, Should heal the lesion within a week or two
- Contact lesion
- Benign whitish, sometimes erythematous or mixed red and white lesion due to chronic, direct contact with a dental restoration (Usually amalgam)
- Diagnosis by removal or the amalgam restoration and replacement. Should result in resolution of the lesion within 2-3 months
- Usually buccal mucosa and borders of the tongue
- Frictional lesion (Frictional keratosis)
- Benign white lesions that is caused by mechanical irritation or friction
- Border of the tongue due to broken tooth or restoration or alveolar mucosa due to toothbrushing or mastication on the oral mucosa
- Homogeneous flat white lesion of the attached gingiva often present in all four quadrants
- Remove causative factor, regression within a few months. Complete disappearance is rare
- Leukedema
- Benign whitish lesion of the oral mucosa
- Tobacco is the main contributing factor
- Rare, mainly adults, often dark skinned
- Veil like, bilateral on buccal mucosa, asymptomatic
- Smoking cessation, may or may not regress
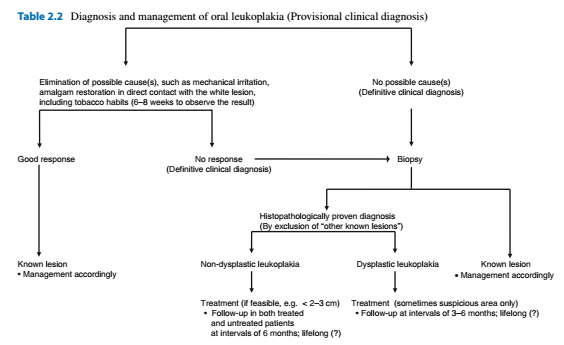
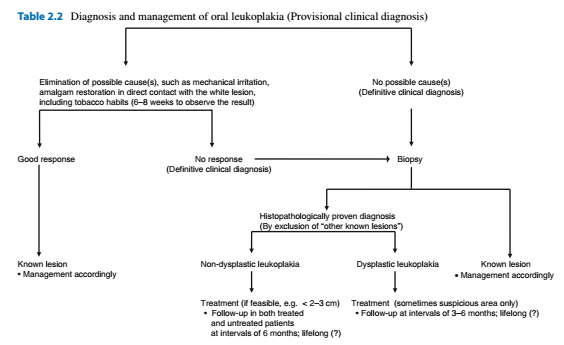
- Leukoplakia
- Clinival diagnosis, white lesions that can't be recognised as any other well defined lesion or condition
- Premalignant 2-3% annually, higher in females, non smoker, >200mm^2, FOM or tongue
- Smokers
- Pain or itching is ominous and may indicate the presence of SCC
- Homogeneous: Uniform flat, thin and white, usually asymptomatic
- Non Homogeneous: Nodular or flat with a mixed white and red discolouration, often burning sensation especially erythroleukoplakia
- Biopsy should be taken every time symptoms are present. In asymptomatic leukoplakias, cease etiologic factors e.g smoking. Wait 6-8 weeks. If unchanged, one or more biopsies should be taken.
- Lichen planus
- May occur along with other mucosas e.g vaginal
- Reticular: White striae (Whickham's striae)
- Erythematous: Most likely to cause symptoms i.e pain and bleeding (in gingival involvement)
- Plaque type (Resembles leukoplakia)
- Ulcerative
- Bullous
- Almost always bilateral, close to symmetrical distribution, Patient usually can't tolerate spicy foods
- Buccal mucosa, gingiva, dorsal tongue. FOM and palate is rare. Gingival involvement should consider vulvovaginal gingiva syndrome
- Characterised by remissions and exacerbations with intervals of several weeks or months of both signs and symptoms
- Many years to lifelong disease. No cure for OLP. Management with corticosteroids.
- Lichenoid lesions
- May be caused by direct anatomic contact with a large amalgam restoration or induced by certain drugs. Drug induced mucosal lesions are much rarer than cutaneous lesions.
- May occur in graft vs host disease
- sometimes difficult to distinguish from leukoplasia, Lupus erythematodes, linear IgA disease, MMP
- Lichen sclerosus
- Flat, pale or whitish changes of the skin and mucosa esp vulva
- Rare involvement of oral mucosa
- Upper or lower lip and rarely tongue or corners of the mouth
- No cure, may regress spontaneously
- Linea Alba
- Benign whitish line on the buccal mucosa at the line of occlusion
- Always bilateral, asymptomatic
- Lupus erythematodes, discoid type
- Scaly, erythematous patches of the skin, mucosa (mainly buccal mucosa and palate)
- May occur in children, more common in women
- Oral lesions may have a lichenoid appearance or present as tiny reddish nodules esp on palate. Often painful and bilateral
- Topical corticosteroids
- Morsicatio
- Benign whitish-yellowish scaly lesion of the oral mucosa caused by habitual biting or chewing. Asymptomatic
- Common, adults
- Almost always bilateral, may occur on the buccal mucosa but also on the borders of the tongue and lips
- No treatment, cease habit, bruxism splint
- White sponge nevus
- Benign, heretitary
- Rare, manifests during childhood
- White, thickened buccal mucosa and border of tongue, usually bilateral.
- No treatment or followup
Comments
Post a Comment
Please leave a comment and let me know what you think or if there are any topics you would like covered in the future