Calcifications in OPGs
Watched a CPD video on OPG calcifications. The main groups were:
-TMJ calcifications
-Sinus calcifications
-Glandular calcifications
-Lymph node calcifications
Why do they occur?
1. Dystrophic calcification: Most common in OPGs, Damaged/degenerating tissue. Often a sign of ageing but can be pathologic
2. Metastatic calcification: Rarest: Increased plasma levels dt metabolic disorder e.g hyperparathyroidism
3. Calcinosis: Vascular disease where there is calcification in the sub-, cutaneous or deep ST. Assoc with collagen vascular disease
4. Other
Where? 3 broad areas
1. Intracranial: Brain, pituitary
2. Maxillofacial: TMJ, Sinus, Salivary glands, lymph nodes
3. Neck: Lymph nodes, ligaments, vascular
Maxillofacial
TMJ:
-Osteophyte fracture: Osteoarthritic changes, breaks off and causes "joint mites" in the joint space
- Ankylosis: Loss in height of condylar neck and change in morphology (loss of outline and hypoattentuating area in the joint space) Rare but can occur after trauma
-Synovial chondramatosis: Growths within the TMJ joint. Unilateral. Can cause displacement over time- Shift in mandible midline. Calcifications in the articular cartilage. Can lead to occlusal changes, fractures in teeth, RCT, Extractions unilaterally.
Maxillary sinus:
- Antroliths: Isolated hyperdensities floating in the ST. Dystrophic calcification from a nidue e.g dead cells in chronic sinusitis or a foreign body
- Tumours: Odontoma, extrinsic sinus problem, Commonly in posterior region where they are complex. Compound in the anterior region
- Chronic sinusitis: Difficult to determine the outline of the maxillary sinus. ST material relatively radioopaque. Sinus material which fills the floor of the maxillary sinus. Tends to be curvolinear and adjacent to the sinus separated by a radiolucent rim. Seen on OPG and confirmed with CBCT
-Fungal sinusitis/Aspergillus: rare fungal disease can be in the sinus. Diffuse sinus border. Often indicates chronic disease process and walls have been compromised
Salivary glands:
Submandibular 80%: Pain and swelling on eating
-Can form ductally (Wharton's duct): singular, unilateral, larger
-Glandular: Less common. Onion skin appearance or punctate and diffuse, Always superimposed over antegonial notch or angle of mandible
Parotid
Sublingual
Lymph tissue in the peritonsillar space (i.e palatine tonsils)
-Calcified tonsils (Tonsiloliths): Not necessarily bilateral. multiple, punctate, almost always superimposed over oropharyngeal space as they are in the parapharyngeal space. Seen in an elderly population where there were no prophylactic removal of tonsils. Associated with chronic recurrent infections, seen intraorally, see mallampatti scoring system for sizing of tonsils. Possible airway reduction, contribution to sleep apnoea. Question of sleep habits, difficulty breathing and uncontrolled BP
Neck calcifications:
Lymph nodes: NOT A NORMAL FINDING and should involve further investigation with minimal being a hx. Common in granulomatous disease:
Sarcoidosis, histoplasmosis (50%)
Tuberculosis/HIV/Aids (6-7%) Tuberculous cervical lymphadenitis
Rarely: Lymphoma, Metastatic thyroid, prostate, breast, OSCC
Usually inferior to the mandible not superimposed. May be affected by patient positioning. Cauliflower shaped i.e bulbous and outside undulations not round and layered like an onion.
Ligamentous calcifications:
Calcified stylohyoid chain: Long, finger like projections, lateral hyperdensity. Can calcify in different patterns anywhere along the ligament. can be related to two syndromes that can mimic TMD (Very rare)
Eagle syndrome: Dysphagia, limited opening
Ernest syndrome: Calcification of the stylomandibular ligament
Laryngeal calcifications: Unusally imaged on the lateroposterior inferior border of the OPG. Physiologic in nature so no follow up. But can be confused with calcified atheroma. Carotid artery is posterior to the pharyngeal space and is a reference for locating these.
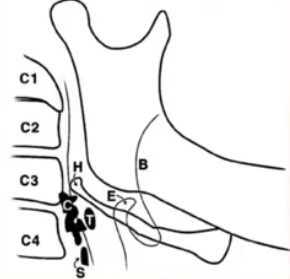
Lateral thyrohyoid ligament-> Calcified triticeous cartilage. Common. Small singular and ricegrain like anterior and immediately inferior to the horn of the hyoid bone. Usually more superior to where carotid artery calcification may occur
Superior Cornu (horn) of the thyroid cartilage: Common and progressive. Entire thyroid cartilage calcifies completely by the age of 70. Boomerang shape. Below carotid artery, around C4
Vascular:
Phlebolith: Rare. Vascular malformations in the venous system. Lymph nodes don't usually calcify at multiple spots. Can occur in the brain, Have they had haemangiomas or and vascular conditions e.g Stephen-Weber syndrome. Tonsillar structures would be smaller and follow the air space. Phlebolithsare associated with low flow lesions i.e Venous capillary, lymphatic malformations cf high flow malformations: Arterial, AV malformations
Medial Arterial calcifications: Not common. Pipe stem, tram line or serpentine calcifications. Usually bilateral, seen in end stage renal disease and diabetes mellitus. Also seen in feet and hands. Referral is needed to internal medicine or vascular specialist
Maxillary artery
Facial artery
Calcified carotid artery atheroma: Crescent shaped/vertical curvolinear radioopacity, single or serial parallel below hyoid, adjacent to C3/4 which corresponds to the bifurcation of the internal and external carotid artery. Asymptomatic, >50 Y.O (2-3%). Post Almost always posterior to oropharyngeal space and anterior to cervical vertibrae. multiple and larger than tonsilolith and more posterior. Confirm this is there: Take another OPG or take a modified Posterior anterior image (Tilt patient's neck up to move mandible out of the way) with lower KVP (Usually visible in lateral neck). Increased risk of stroke if no previous history of CVD or BP is >140 and not on medications for BP or heart disease.
-TMJ calcifications
-Sinus calcifications
-Glandular calcifications
-Lymph node calcifications
Why do they occur?
1. Dystrophic calcification: Most common in OPGs, Damaged/degenerating tissue. Often a sign of ageing but can be pathologic
2. Metastatic calcification: Rarest: Increased plasma levels dt metabolic disorder e.g hyperparathyroidism
3. Calcinosis: Vascular disease where there is calcification in the sub-, cutaneous or deep ST. Assoc with collagen vascular disease
4. Other
Where? 3 broad areas
1. Intracranial: Brain, pituitary
2. Maxillofacial: TMJ, Sinus, Salivary glands, lymph nodes
3. Neck: Lymph nodes, ligaments, vascular
Maxillofacial
TMJ:
-Osteophyte fracture: Osteoarthritic changes, breaks off and causes "joint mites" in the joint space
- Ankylosis: Loss in height of condylar neck and change in morphology (loss of outline and hypoattentuating area in the joint space) Rare but can occur after trauma
-Synovial chondramatosis: Growths within the TMJ joint. Unilateral. Can cause displacement over time- Shift in mandible midline. Calcifications in the articular cartilage. Can lead to occlusal changes, fractures in teeth, RCT, Extractions unilaterally.
Maxillary sinus:
- Antroliths: Isolated hyperdensities floating in the ST. Dystrophic calcification from a nidue e.g dead cells in chronic sinusitis or a foreign body
- Tumours: Odontoma, extrinsic sinus problem, Commonly in posterior region where they are complex. Compound in the anterior region
- Chronic sinusitis: Difficult to determine the outline of the maxillary sinus. ST material relatively radioopaque. Sinus material which fills the floor of the maxillary sinus. Tends to be curvolinear and adjacent to the sinus separated by a radiolucent rim. Seen on OPG and confirmed with CBCT
-Fungal sinusitis/Aspergillus: rare fungal disease can be in the sinus. Diffuse sinus border. Often indicates chronic disease process and walls have been compromised
Salivary glands:
Submandibular 80%: Pain and swelling on eating
-Can form ductally (Wharton's duct): singular, unilateral, larger
-Glandular: Less common. Onion skin appearance or punctate and diffuse, Always superimposed over antegonial notch or angle of mandible
Parotid
Sublingual
Lymph tissue in the peritonsillar space (i.e palatine tonsils)
-Calcified tonsils (Tonsiloliths): Not necessarily bilateral. multiple, punctate, almost always superimposed over oropharyngeal space as they are in the parapharyngeal space. Seen in an elderly population where there were no prophylactic removal of tonsils. Associated with chronic recurrent infections, seen intraorally, see mallampatti scoring system for sizing of tonsils. Possible airway reduction, contribution to sleep apnoea. Question of sleep habits, difficulty breathing and uncontrolled BP
Neck calcifications:
Lymph nodes: NOT A NORMAL FINDING and should involve further investigation with minimal being a hx. Common in granulomatous disease:
Sarcoidosis, histoplasmosis (50%)
Tuberculosis/HIV/Aids (6-7%) Tuberculous cervical lymphadenitis
Rarely: Lymphoma, Metastatic thyroid, prostate, breast, OSCC
Usually inferior to the mandible not superimposed. May be affected by patient positioning. Cauliflower shaped i.e bulbous and outside undulations not round and layered like an onion.
Ligamentous calcifications:
Calcified stylohyoid chain: Long, finger like projections, lateral hyperdensity. Can calcify in different patterns anywhere along the ligament. can be related to two syndromes that can mimic TMD (Very rare)
Eagle syndrome: Dysphagia, limited opening
Ernest syndrome: Calcification of the stylomandibular ligament
Laryngeal calcifications: Unusally imaged on the lateroposterior inferior border of the OPG. Physiologic in nature so no follow up. But can be confused with calcified atheroma. Carotid artery is posterior to the pharyngeal space and is a reference for locating these.
Lateral thyrohyoid ligament-> Calcified triticeous cartilage. Common. Small singular and ricegrain like anterior and immediately inferior to the horn of the hyoid bone. Usually more superior to where carotid artery calcification may occur
Superior Cornu (horn) of the thyroid cartilage: Common and progressive. Entire thyroid cartilage calcifies completely by the age of 70. Boomerang shape. Below carotid artery, around C4
Vascular:
Phlebolith: Rare. Vascular malformations in the venous system. Lymph nodes don't usually calcify at multiple spots. Can occur in the brain, Have they had haemangiomas or and vascular conditions e.g Stephen-Weber syndrome. Tonsillar structures would be smaller and follow the air space. Phlebolithsare associated with low flow lesions i.e Venous capillary, lymphatic malformations cf high flow malformations: Arterial, AV malformations
Medial Arterial calcifications: Not common. Pipe stem, tram line or serpentine calcifications. Usually bilateral, seen in end stage renal disease and diabetes mellitus. Also seen in feet and hands. Referral is needed to internal medicine or vascular specialist
Maxillary artery
Facial artery
Calcified carotid artery atheroma: Crescent shaped/vertical curvolinear radioopacity, single or serial parallel below hyoid, adjacent to C3/4 which corresponds to the bifurcation of the internal and external carotid artery. Asymptomatic, >50 Y.O (2-3%). Post Almost always posterior to oropharyngeal space and anterior to cervical vertibrae. multiple and larger than tonsilolith and more posterior. Confirm this is there: Take another OPG or take a modified Posterior anterior image (Tilt patient's neck up to move mandible out of the way) with lower KVP (Usually visible in lateral neck). Increased risk of stroke if no previous history of CVD or BP is >140 and not on medications for BP or heart disease.

Comments
Post a Comment
Please leave a comment and let me know what you think or if there are any topics you would like covered in the future