A post on bruxism (Part 4)
From Contemporary oral medicine 2019
The management of SB aims mainly to reduce the damage and consequences of SB rather than reducing the muscle activity.
The management of SB aims mainly to reduce the damage and consequences of SB rather than reducing the muscle activity.
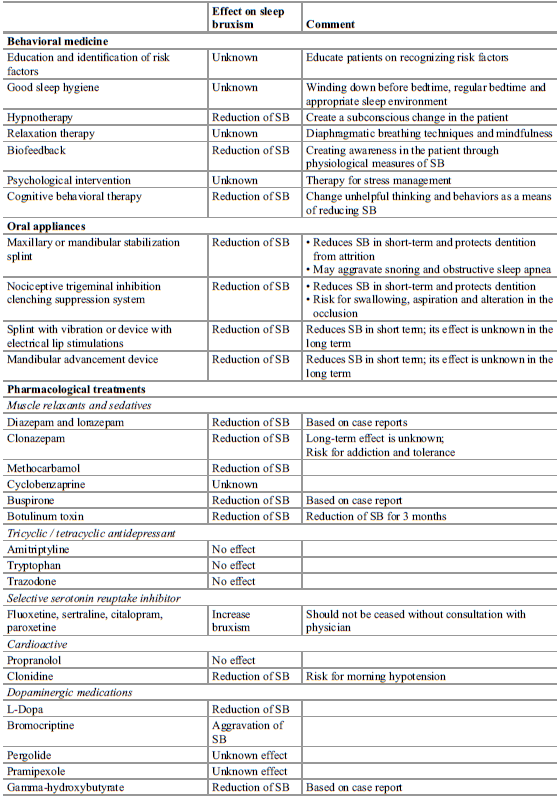
- Behavioural medicine: Most of these concepts are based on expert opinion and lack long term results. Avoidance of triggers such as cigarettes, caffeine, alcohol and illicit drugs can be beneficial. Habit awareness and reversal techniques for AB will reduce attrition of the dentition. Relaxation techniques, good sleep hygiene and hypnotherapy may be useful for SB and AB.
- Oral appliance: First line therapy for SB associated with TMD. Mechanism of action is under unresolved debate. Current evidence suggests that oral appliances decrease SB transiently for the first 2 weeks of wear with SB continuing in the long term. Changes to occlusion may occur as a side effect and may not be tolerate by those with an active gag reflex. The use of maxillary stabilisation splints may increase the AHI and risk for snoring due to reduced tongue space. Therefore it is suggested in SDB comorbid patients a mandibular stabilisation splint is used. Anterior splints such as the NTI are occasionally used of SB and TMD. It is hypothesised that short term use reduced EMG activity and alters prioprioceptive input of patients enabling them to be more aware of daytime parafunction. Long term outcomes are unknown and there is a risk of swallowing or aspiration during sleep. Mandibular advancement appliances can be used to treat snoring and mild-moderate OSA and can be used for SB. It is theorised that improvements are related to improved airway patency which reduces the reactive mechanism of SB in patients with OSA. Another theory is the protrusive position being a starin on the mandible reducing the capacity for SB. These splints may also reduce morning headaches in patients with low levels of RMMA.
- Pharmacological treatments: There are some medications that may work centrally to decrease or increase SB activity. These typically involve the dopimanergic, seretoninergic and adrenergic systems effect on oromotor activity. However, medications are rarely used in clinical practice for the treatment of SB as there is little evidence for their efficacy and safety. Medications should only be considered in cases of symptomatic TMD secondary to severe SB.
- Clonazepam: A benzodiazepine with anxiolytic, hypnotic, anticonvulsive and muscle relaxant properties. A dose of 1mg has been found to reduce SB by 40% but this has failed to be repeated. Long term efficacy is unknown and there are side effects of sleepiness, tolerance and dependence.
- Antidepressant medications: Low dose TCAs e.g amitryptaline do not reduce SB and SSRIs e.g setraline or citalopram can increase tooth grinding and clenching.Another SSRI, Busiprone may reduce secondary SB activity in the short term.
- Antihypertensive medications: Beta blockers such as propanolol have no effect on SB. Short term use of clinidine 0.3mg has been found to reduce SB activity by 60% which may be due to blunting of the activation of the autonomic-cardiac system involved in the physiology of SB. However, this high dose was assocated with severe hypotension on waking. A 0.15mg dose was associated with a 30% reduction of RMMA and less side effects.
- Botulism toxin: First line therapy for head and neck movement disorders. It is used routinely for the treatment of primary SB and secondary SB secondary to a movement disorder. Botox is a neurotoxin produced by Clostridium botulinium. It interferes with neural transmission by blocking the release of acetylcholine, the principle neurotransmitter at the neuromuscular junction causing muscle paralysis.Botox injected into the masticatory muscles can decrease EMG activity during sleep and awake clenching however doesn't have an effect on the generatory of RMMA. Its effect only lasts for 3-4 months and will need to be repeated.
Comments
Post a Comment
Please leave a comment and let me know what you think or if there are any topics you would like covered in the future