Crown impressions on deep subgingival margins
Today I reattempted an impression on a crown preparation with a deep subgingival margin. It was a very heavily filled lower molar with a subgingival buccal GIC restoration. I knew that the tooth was compromised but had not placed any of the restorations so I didn't know how extensive the restorations were and it was not obvious radiographically. When I removed all the restorations and caries to place a core, I was surprised how deep gingingival the mesiobuccal restoration went. It is hard to tell on the photographs but the midbuccal and mesiobuccal margin was about 4-5mm below the gingival margin. Halfway through the procedure, I didn't many places to go other than to keep going ahead with the plan and see how it turned out. What was surprising was how non inflamed the gingiva was preoperatively despite having such a deep margin. Partly this may be due to the patient's thick gingival biotype or partly it may be due to the margin being buried so deep that the inflammation was too far from the external tissue surface to be obvious. I am not sure how valid these theories are but they are the things that came to mind.
I tried multiple tips and tricks to try and get isolation for the core buildup but was struggling to stop the bleeding. The inflammation that had previously been subtle was very obvious due to the tissue trauma from removing the fillings and exposing the inflamed sulcus. I tried retraction cord and hemostatic agent, PTFE tape retraction, cotton pellets soaked in hemostatic agent with pressure and a tofflemire with the retainer on the lingual. None of these were successful in perfectly successful but after some time I had controlled it enough to place a new GIC core. I completed the crown preparation with margins in solid tooth. Lacking time to take an impression I cemented a temporary crown and brought the patient back a couple of weeks later to attempt impressions.
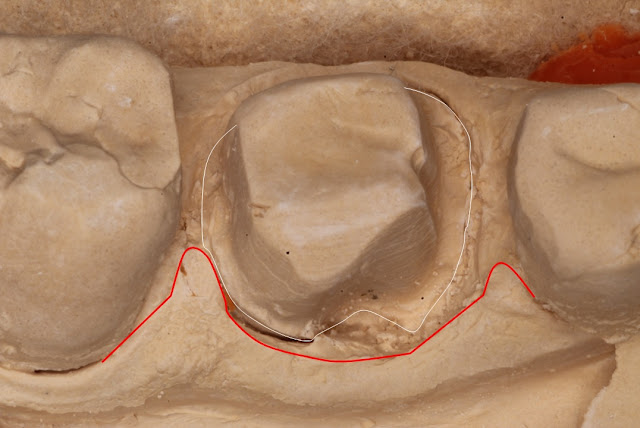
The impression appointment went similarly shocking as I struggled with tissue fluid control and retraction. The patient's tissue attachment was clearly below the margin but there wasn't much sulcus to fit retraction cord so the cord pretty much took up all the sulcus space and was sitting equigingivally rather than gingival to the sulcus. I assume my temporary wasn't smooth enough or fitting well enough or I hadn't waited long enough for tissue healing but the tissue was quite inflamed and was bleeding a lot during manipulation. When I removed the second cord, the tissue was bleeding onto the prep but I went ahead and took the impression anyway. It looked alright at the impression stage but wasn't so great once poured up (Figure 1). The impression was inadequate for a well fitting crown so it had to be redone.
The patient had a lot of personal commitments and was unable to come back for a re-impression appointment for a number of months. The initial temporary crown had cracked and was replaced at the initial impression appointment. At that appointment I paid special attention to getting the occlusion right and margins well fitting and smooth. When the patient returned back today after approximately 3 months, the temporary crown was surviving well and the tissue looked absolutely perfect around the deep margins. The sabbatical was a double edged sword as I had been dreading the appointment today the whole time as I assumed I would struggle and not be able to achieve a good impression and that I was not skilled enough to achieve success in this case. The benefit of the time off was it gave me time to improve my skills and think of strategies to overcome the difficulties of this case.
In the past few months I found myself doing a fair bit of equigingival and subgingival class V restorations and have increasingly found that I was using gingival retraction cord. In the past, PTFE retraction was my main form of retraction but I have started to use cord more and more lately. I have started to get the feel of handling it and knowing what pressure to apply and in what direction it is needed to enter and stay in the sulcus. As far as I could tell, the impression went quite well today (Figure 2).
The things that went different this appointment that all added to a better result were:
- I had left more than enough time for the tissue to heal after the trauma of core replacement and crown preparation
- I had made a well fitting and smooth temporary crown that was conducive to tissue healing
- I placed cord better and atraumatically. My technique for placing cord in a deep margin is to use the tooth surface as a guide to place the cord down. I slide my cord packer down the axial wall of the prep pushing the cord along the tooth surface till I hit the horizontal margin then slide along the margin into the tissue putting horizontal pressure away from the tooth and vertical pressure down into the sulcus. Before I wouldn't use the tooth as a guide and would end up pushing my instrument deep into the tissue causing more trauma. When placing the horizontal and vertical pressure on the cord, I held this pressure for a couple of seconds before lifting the packer. This is because gum tissue is elastic and if you take the pressure off too early, the tissue will bounce back and push the cord back out.
- For my initial cord I used a 000 size and buried it into the tissue. This stays in to block gingival crevicular fluid and to hold hemostatic agent in the tissue. I used a first cord that was slightly too long and overlapped the excess cord in the distal area so that there was extra cord in the area where I had failed to capture the margin in the first instance and potentially as the cord was overlapped it would be less likely to be pulled out when the second cord was removed.
- I used a larger second cord for this impression appointment. I think in the initial impression I used a size 1 for the second cord but considering the thick biotype and the amount of retraction I needed I used a size 3 cord today. This is larger than any cord I've ever used but it was very effective and the risk of recession is low considering the patient's biotype. The size 1 cord would have completely entered the sulcus in some areas especially the distal. I am used to packing my second cord all the way into the sulcus but this is counter productive as the aim is to produce horizontal retraction at the gingival margin and if the second cord disappears into the sulcus then at the gingival margin, the tissue will fold back over the cord towards the tooth. The cord needs to be large enough to displace the margin away and therefore should be visible all the way around the prep. In this case, even the size 3 cord fell into the sulcus on the distal so I packed a second cord over this until there was retraction of the gingival margin. If the second cord goes too deep into the sulcus there is risk that some part of it sinks under the first cord and pulls the first cord out when the second cord is removed. This happened to me quite often in the past and is very frustrating as it will cause tissue bleeding when you least want it.
- I waited long enough for tissue retraction and hemostasis to take place. If I don't look at the clock and set a time before I can touch the cords again, I will be tempted to touch the cords early and there will not be enough retraction and the tissues will start bleeding again. The cords need enough time to displace fluid from the tissues and the hemostatic agent and cord pressure needs enough time for the bleeding to stop.
- I washed away any blood and fluid and reapplied hemostatic agent to the cord. This removed any blood clots on the prep and tissue that may be torn off when the second cord was removed. As the second cord was correctly sticking out of the sulcus, it could suck up the new application of hemostatic agent. I waited 15 minutes and let the patient show me pictures of her daughter's engagement party before taking the cords out. This is a good time for yourself and the patient to rest. Adding 15- 30 minutes to your appointment time to reduce stress and increase your chance of a successful result isn't too costly at all especially if it reduces the need to re-impression which wastes more time and materials. The one place I didn't wait long enough was at the distal margin where I added the extra layer of size 3 cord. This spot had about 5 minutes of waiting before removal and was the only place I had any bleeding on removing the second cord.
- I wet the cords with water before removing them. This reduced the risk of the second cord sticking to the first cord and pulling it out or sticking to the tissues causing bleeding.
- The impression technique was mostly the same from then on out but the tissue management made all the difference here. One point I refined was to remove the tip of the impression gun from the mass of light body at a point on the adjacent tooth as the tip removal may introduce a bubble as the material falls off the withdrawing tip and folds back onto the tooth. You would much rather this be on a neighboring tooth or on the tissues in the vestibule where it won't interfere with the prep.
The temporary crown was extremely retentive due to the tall height of the prep having lots of retention due to the subgingival margin and I had to section the crown off every time. I spent a lot of attention into the temporary crown today(Figure 3) and have a few points to note down.
 |
| Figure 3: The temporary crown today. The white line approximates the gingival margin and the black circle indicates the desired contact area |
- The material continues to set after it's initial set phase. I made the temporary in the putty key, took it out with the putty key and left it on the bench untouched while I took my upper alginate and bite registration. This is to give it extra time to harden and prevent distortion upon removing it from the putty key and handling it.
- When trimming the temporary crown I use a diamond fissure bur with no water and with high speed suction to cut off the bulk below the margins. The less accurately the putty key fits, the thicker and smaller the flash will be. Then more accurate the putty key, the thinner and more spread out the flash will be.
- Just like the impression material has to extend vertically past the horizontal margin, the temporary crown will have excess past the horizontal margin. When viewed from below, you should see a distinct transition from the horizontal part of the margin tot he vertical excess. This is the finish line for the temporary crown and I use a large red rough soflex disc at a flat angle to trim the temporary until this point.
- The margin is where you are most likely to get an air bubble when seating the putty key as the air is displaced by the pressure of the seating putty and bubbles are forced into any nook that isn't smooth. To get around this, after filling the putty key, I quickly cover the tooth in temporary crown material using a similar technique with the light body keeping the tip buried in the mass of material. This ensures that the margins are completely covered with material when the key is seated. There is a chance to introduce bubbles at the interface between the material on the tooth and the material in the putty key but this is less likely to be at the margin and more likely to be at a smooth surface that can be repaired or of no consequence.
- The external surface of the temporary near the tissues (Figure 3) needs to be extremely highly polished. I spend a fair bit of time getting this area super smooth to allow good tissue response.
- When trimming the excess of the temporary crown material away, to ensure a good contact point, the position of the intended contact area (Figure 3) should not be touched at all. This is because the material flowed into the available space until it contacted the adjacent tooth so technically if all the area around this position is trimmed then the contact points will be perfect. You can mark this area with a pencil or marker to ensure that it is not adjusted. Some leeway is present with material distortion, shrinkage and warping and in this case the contacts were slightly tight so I lightly adjusted them with a disc until the temporary crown seated well.
- In the past, with a super retentive prep, I tried the crown on with a snap fit and had massive amounts of trouble getting it back off. The problem is that there is no die spacing and the intimate fit of the temporary can lock into microscopic undercuts or into surface roughnesses and the resistance and retention form can prevent removal. This particular case I had to section the temporary off last visit after trying it in and make a new temporary crown. I probably could have left it on without any temporary cement but I hadn't finished polishing the crown. This time, I completely finished polishing the crown before attempting a try in. I didn't try the crown till it was 100% seated, I gently pressed down to test the tightness of the contacts, took it off to adjust and when i could get it 90% seated knowing that I had gotten past the tightest part of the contact, I took it off and cemented it. In my mind I was quite sure there hadn't been any significant distortion of the temporary crown at it had come out fine with the putty key and I had waited for it to set properly before handling it. I compared the cost-benefits of two situations: 1. If I had attempted to cement the temporary crown and it didn't seat 100% down, it would take me less time to remove it before the cement had set, remove the cement from the tooth and temporary crown and adjust it to fit compared to 2. doing a dry test for the temporary crown till it was 100% seated and then struggling to get it off like last time, having to section it off and remake a new temporary crown (as I had spent about 10 minutes on it by this time).
All in all I think it was a very successful appointment today and much better and smoother than I was dreading. I sincerely hope that it turns out well when the impression is poured and I know there will be similar challenges with tissue management at the cementation stage. Hopefully I will be able to update the situation as it progresses but all in all there were many learning points I took away from today and I will certainly be trying to refine my techniques further in the future as I learn more from others and from my own practice.

Comments
Post a Comment
Please leave a comment and let me know what you think or if there are any topics you would like covered in the future